The Disillusionment Phase of the Pandemic Is Upon Us

Image: Shutterstock by Iryna Kalamurza and Jane Sherman
This may come as a surprise, but the coronavirus pandemic had a “honeymoon phase.” At least according to a recent forecast published by the Washington State Department of Health. The report, authored by Washington’s Behavioral Health Strike Team, predicts how the pandemic will affect the mental and emotional health of Washingtonians, along with substance use, crime, domestic violence, and other social or psychological problems.
The forecast features a graph (yes, another Covid-related curve) that maps out a community’s typical emotional response to disaster. First comes a subtle dip in mental health with the threat of an impending crisis. Then, about a month and a half after a disaster, there’s an upward spike—the honeymoon—as people band together to overcome what’s perceived as a temporary setback. According to Dr. Kira Mauseth, co-lead of the Strike Team and a senior instructor of psychology at Seattle University, it’s a period characterized by a desire to help one another. “That’s when community cohesion is at its highest, and that’s when optimism is at its highest,” explains Mauseth.
After a while, though, mental resilience wanes. The novel coronavirus loses its novelty (remember when we made toilet paper jokes?). As we enter into fall, the Strike Team warns, what once felt like an opportunity for global connection has transitioned to a disappointing new normal. Welcome to the disillusionment phase.
Disillusionment begins to set in when cortisol—our principal stress hormone—overwhelms the brain. “Our brains are constantly scanning for threats,” explains Mauseth. “They’ve been doing that for six months and they’re tired.… When people are tired, they can’t regulate their emotional responses as effectively.”
During the disillusionment phase, mental health usually bottoms out about six to nine months after the initial disaster. The Strike Team deems mid-March the beginning of this particular disaster, so we’re likely in for another rough couple months.
The Strike Team predicts a rise in the number of Washingtonians reporting experiences of anxiety or depression as well as deaths by suicide and drug overdose (suicide rates often correlate with unemployment rates, too). The report notes that shifts in behavioral health disproportionately impact people of color, along with low-income community members. And the loss of daylight as we enter fall and winter could worsen feelings of disillusionment for Washingtonians, whether or not they’ve experienced symptoms of Seasonal Affective Disorder (SAD) in the past.
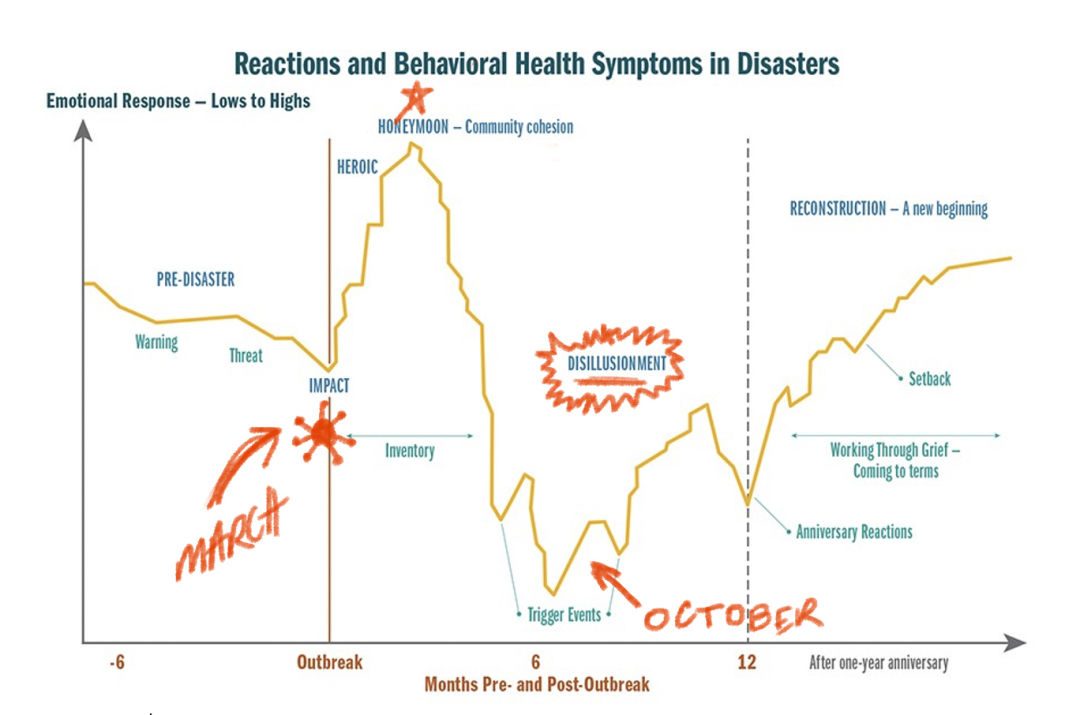
Phases of reactions and behavioral health symptoms in disasters. Adapted from the Substance Abuse and Mental Health Services Administration (SAMHSA).
Image: Courtesy SAMHSA and Jane Sherman
The Strike Team uses a graph that reflects community responses to all kinds of disasters. Mauseth herself has worked with refugees and earthquake survivors. Psychological responses to Covid-19, she says, will likely follow the same pattern as those to other events, but the types of psychological struggles may differ. With an event like 9/11, or an earthquake, where people face immediate threats to their lives, PTSD is a common response. With the pandemic, in contrast, social isolation has led to an increase in depression and anxiety.
But even those who don’t experience clinical levels of depression or anxiety will likely continue to feel some kind of psychological burden from the pandemic. “No single brain or body is immune to where we are in the disaster recovery cycle,” says Mauseth. Common responses during the disillusionment phase include difficulty focusing or remembering details, along with a shorter temper and tendency to express anger and frustration toward others.
It’s not exactly cheerful news, but Mauseth says it’s important that we prepare ourselves—both individually and as a community—for what lies ahead. “I would focus on those elements of resilience: hope, adaptability, flexibility, purpose, and connection,” Mauseth says. “That’s what we need to focus on right now: being creative in finding ways to meet those needs.” As for how we might do this, the Department of Health provides some recommendations for different groups.
In most disasters, Mauseth says, people generally return to their baseline for mental and emotional health about 12 to 16 months following the initial event. With Covid-19, she says, this could take a little longer—there’s more than infrastructure that must be rebuilt. But even if we’re still wearing masks two years from now, that doesn’t mean the recovery phase is out of reach. It just requires embracing a flexible, adaptive approach. “If you hang on and you say, ‘It has to be the way it was; I’m not going to see my family or I’m not going to see my friends until it can be exactly like it was in January or February,’ well, you’re going to have a long wait. When people are adaptive, then they’re likely to recover more quickly.




