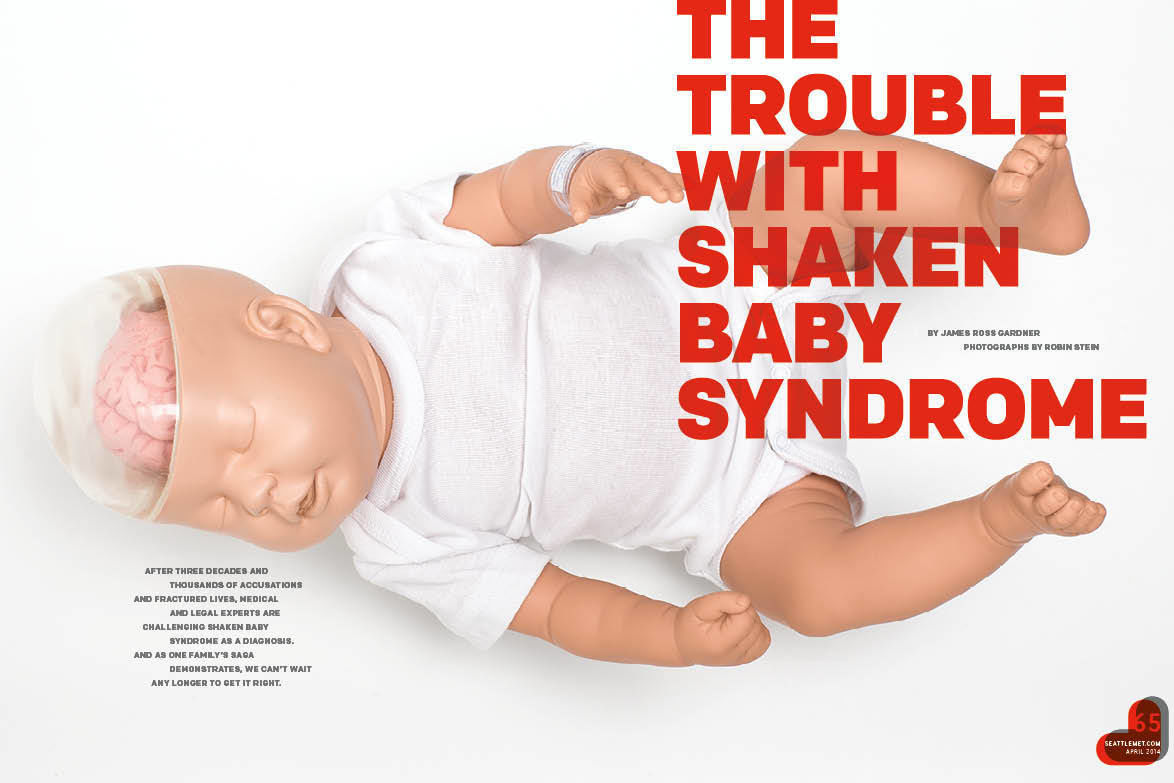
The Trouble with Shaken Baby Syndrome
BEFORE ROBYN FELIX FEARED EVERY UNFAMILIAR CAR THAT wheeled down her street, or hid with the babies at the back of the house with the lights off, or fell into the habit of washing the same dishes over and over for hours, there came the sound at the door.
Knock isn’t the right word. Robyn would later think of the pounding on the door that jerked her and her husband Nathan awake that Friday in late November as an evil come to pull their lives apart.
Nicholas, their infant son, had already endured three days of medical exams and now lay in a bed 50 miles away with what doctors said were rib fractures and retinal hemorrhaging. It was hard for Robyn, a nurse at Swedish Medical Center, and Nathan, a medical assistant at Country Doctor Community Clinic, to fathom worse. Yet there it was—bam, bam, bam—the harbinger of all that would befall the family, and it echoed through their Everett home at 10:30pm.
In the doorway stood a handful of Snohomish County sheriff’s deputies flanking a woman who introduced herself as a caseworker from Child Protective Services. They’d come for Eliana, the couple’s one-and-a-half-year-old daughter. “Do you have identification?” Robyn asked the woman. No. “A court order?” The largest deputy in the group, maybe six-five, 250 pounds, placed his boot over the doorsill. I’m the court order, he said. They weren’t leaving without Eliana. Robyn scanned the street. At least five patrol cars lined the curb. Every home on the street glowed, the silhouettes of onlooking neighbors framed in the windows. After a 30-minute standoff—the deputies demanding entry into the house, the Felixes refusing—and after tearful phone calls to friends for advice, Robyn woke Eliana in her crib, bundled her, and passed the toddler to the caseworker. The child cried out for Nathan—“My daddy! My daddy!”—and disappeared into the backseat of the caseworker’s car.
One of the deputies turned to Nathan, who stood barefoot in the doorway in his T-shirt and pajama bottoms. Can you come out to my car? We have paperwork for you to sign. As soon as Nathan’s feet hit the public sidewalk, the deputies cuffed him. They had probable cause, they said, that he’d assaulted a child. Based on statements made at Seattle Children’s hospital, authorities believed Nathan had savagely shaken his newly adopted son—whom they had removed from his custody 27 days earlier—and that he posed an imminent risk to Eliana’s safety.
Robyn watched the cars roll out of the neighborhood. It was near midnight. Her husband and two of her children had been taken from her. Half an hour later, more patrol cars arrived.
Things really were about to get worse.
The symptoms that doctors at Seattle Children’s said they’d discovered when Robyn and Nathan Felix brought in their three-month-old son Nicholas on October 21, 2008, a month before Nathan’s arrest, are commonly associated with what’s called shaken baby syndrome. First identified in the 1970s, SBS is diagnosed via a triad of symptoms: retinal hemorrhage (bleeding at the back of the eye), subdural hematoma (blood gathered between the outermost layer of the brain and the lining between the brain and the skull), and cerebral edema (excess fluid in the brain). Medical professionals have long maintained that a parent or caretaker, exasperated by an infant or toddler who won’t stop crying, shakes the child, causing the symptoms, which can lead to permanent brain damage or death.
The National Center on Shaken Baby Syndrome in Farmington, Utah, asserts that some 1,400 children in the U.S., usually between three and eight months old, are severely injured or killed from shaking every year. The NCSBS’s educational programs—including DVDs and booklets for new parents and training materials for staff to help identify symptoms of shaken baby syndrome—are distributed in more than 2,000 hospitals in 49 states, including 38 in Washington. Seattle Children’s has long had a relationship with the center, garnering a grant in 2008 for the implementation of NCSBS’s programs in area hospitals.
The symptoms medical professionals look for, identified via brain scans and basic eye exams, have functioned as a kind of prosecutorial slam dunk for decades. A case analysis issued in 2007 put the conviction rate of those accused of SBS at 95 percent, 90 percent of which resulted in life sentences, notes Deborah Tuerkheimer, a DePaul University law professor and author of the just-published book, Flawed Convictions: “Shaken Baby Syndrome” and the Inertia of Injustice.
SBS has been used, Tuerkheimer writes, to establish “each element of the crime charged: that the act of shaking caused the infant’s injury or death; that the shaking was sufficiently violent to evince the mental state required for guilt; and that the person who shook the baby was the defendant.” Put more bluntly, she recently told me, SBS comes “as close as one could imagine to a medical diagnosis of murder.”
That’s changing.
A number of reexamined cases in recent years—aided by new technology and debate among medical experts—have put proponents of the SBS hypothesis on the defensive. Ernie Lopez, who was serving a 60-year-sentence for shaking an infant in his care to death, is now free, thanks in part to the work of retired Seattle lawyer Heather Kirkwood. So is Audrey Edmunds, a woman charged with the murder of a child in her care in the 1990s.
Yet even if they’re ultimately absolved of any wrongdoing, those suspected of SBS are left to pick through the debris of their former lives: loss of employment, financial ruin, the stigma of having been labeled a child abuser.
Over the course of the past year I have contacted Washingtonians who’ve either been acquitted of SBS or whose cases showed sufficient reason for the possibility of exoneration. And in nearly every instance, they either refused to speak to me or asked that any identifying biographical details be left out of my account.
Robyn and Nathan Felix were the exception.
On that Friday night in November 2008, Robyn told me, after the procession drove off with her daughter and husband, a new set of cars pulled up to the curb. This time a deputy presented a warrant to enter the house. Inside, the detectives pulled open kitchen drawers, rummaged through mail, and snapped photographs of the master bedroom and every bathtub in the home.
All the while Robyn couldn’t help thinking about how Child Protective Services had been so convinced that her husband had shaken Nicholas—and how they said that Nathan had better admit to doing something wrong before things got out of hand.
Ten miles away, a detective at the Snohomish County jail read Nathan Felix his Miranda rights. Stripped of his pajamas, Nathan donned a striped jail uniform and entered a cell. He heard the guards talk about placing him in solitary confinement. For his own protection, they said. Inmates aren’t too kind to child abusers. The door slammed shut. The thought weighed so heavily on the 38-year-old that once he had cycled through the anger—aimed at the cops, CPS, and the doctors at Seattle Children’s—he sobbed. He crumpled on the bed of his cell and he wept.
Had he experienced worse? He’d seen worse. Three tours in Afghanistan as a medic—men perforated by enemy bullets, limbs claimed by IEDs. That he’d even gotten that far was its own kind of miracle, the result of a coin toss against fate in which the quarter fell—sometimes—in Nathan’s favor.
Born in 1970 in Knoxville, Tennessee, and put up for adoption by his birth mother, Nathan was an orphan until age one. The first miracle came in the form of Robert and Jacqueline Felix, a married couple who rescued the toddler and raised him with three other adopted siblings in Billerica, Massachusetts. Traditional Roman Catholics, the Felixes were strict but compassionate, instilling in Nathan a strong sense of empathy, a love of learning, and above all, perhaps because they were a multiracial family—Robert and Jacqueline were white; Nathan is part black—open-mindedness.
He enlisted in the Army and, as a linguist and medic, volunteered for the NATO-led mission in Bosnia-Herzegovina in the mid-1990s. By 9/11 he had switched to the Air Force Reserves and subsequently flew in missions in the Middle East.
While stationed at Fort Lewis, Nathan fell in love with the Pacific Northwest, and at Community Health Centers in Lynnwood, where he began work as a medical technician in 1999, he fell in love again. Had anyone walked into the CHC break room back then they might have spotted Nathan, then in his early 30s, lunching with Robyn Roldan, a registered nurse and single mother in her early 40s. Miracle number two.
He was too young for her, she thought at the time, but what a catch. Debt free, good job, handsome—she kept trying to set him up with her friends. With each failed date, the two grew closer and closer. They became a couple in 2001 and married in September 2004. Nathan used his savings for a down payment on a house: five bedrooms and 2,890 square feet in Everett, plenty of room for the newlyweds, Robyn’s three sons from a previous marriage, and the children the couple hoped to have together.
Nathan, Robyn’s friends and family observed, was a natural at parenting. When Robyn’s son Ian, then in eighth grade, swiped the keys and took the family car for a late-night summer joyride, the kid got caught and thought he was toast. Instead, his new stepfather patiently sat him down and explained what it meant to be a responsible man. You’re not licensed, you’re not insured, and you could have hurt someone or yourself, Nathan said. He added that while Ian and the car were AWOL he wasn’t nearly as angry as he was worried for Ian’s safety.
Eager to have children together, Nathan and Robyn sought the help of fertility specialists. Robyn miscarried 11 times—in one case she nearly died—before they decided to adopt. They took out a second mortgage on their home to pay $25,000 for a private adoption and became emotionally invested in one unborn child only to have the birth mother change her mind.
Finally, the adoption agency called with a special case. The birth mother worked as a prostitute and battled drug addiction, but would the Felixes consider adopting her baby girl? Nathan and Robyn didn’t hesitate. They traveled to Kansas in June 2007 to be at the hospital when Eliana was born. When the nurse brought the infant out of the operating room, Robyn thought, “I must be dreaming.” She’d waited for a baby girl for so long. “I knew from the minute they put her in my arms that I was meant to be her mother and she was meant to be my daughter,” she says. “It was instant.”
Eliana had been home for four months when the Felixes received another phone call from the adoption agency. Eliana’s mother was pregnant again, this time with a boy. The decision didn’t come quite as easily, but the couple felt strongly that the siblings should grow up together. For the second time they scraped together enough money for an adoption (Nathan cashed out his retirement, Robyn liquidated her assets) and they awaited the baby’s due date. But because of the mother’s health and lifestyle there were complications: Nicholas was born in July 2008 via an emergency C-section, nearly a month premature. Robyn and Nathan flew to Kansas to be at his side.
“He was hooked up to all kinds of tubes,” Robyn recalls. “I couldn’t hold him and hug him and love on him. Part of me thought he might not survive.” They stayed in Kansas for 11 days, then brought Nicholas home to Everett, where he wailed incessantly, from the moment Robyn stopped feeding him until it was time to feed him again.
Again, Nathan was a natural. “When the rest of us, including Robyn, couldn’t calm Nicholas down, we would hand him to Nathan, who could always soothe him with his magic touch,” the Felixes’ family friend, Athena Wright, would later note in an affidavit. “He had a special way of holding him, more or less horizontal, and he would either hold him like that, or he put him on the bed, plumping pillows around him, so that he was almost in the same position. It always worked when Nathan did it.”
To rule out meningitis, on October 15 the Felixes took Nicholas to Group Health in Bellevue for a lumbar puncture. Robyn couldn’t watch. In the examination room, where a technician tried to insert the needle, “Nathan stayed with Nicholas, but I left. It was too hard to watch them try to position him and he kept crying. I went out into the hall, thinking that the glass door would give me some barrier, but I could still hear him. The quality of his cry started to change, and he started to sound more like a wounded animal and less like a newborn baby.”
The procedure dragged on for 45 minutes, with Nicholas flailing his limbs and the technician changing needles. Unable to bear it any longer, Robyn told a nurse in the hall she wanted to call it off. When they got home Robyn looked under the bandage, which was soaking with what looked like spinal fluid, and discovered five clearly defined puncture holes, three on one side of his spine, two on the other. “Holy cow,” Robyn thought, “no wonder he was screaming so much.”
Worse, Nicholas began to vomit violently. “He was projectile vomiting,” Nathan says. So they checked him into Seattle Children’s hospital for observation.
A consultation with a dietician zeroed in on a protein allergy. When they switched to an amino acid–based formula, Nicholas took an immediate turn for the better. He stopped crying and didn’t have so much as a wet burp.
During the three days that Nicholas stayed at Children’s, he underwent scans that revealed a retinal hemorrhage, subdural hemorrhage, cerebral edema, and small fractures on three ribs.
On October 24, a doctor pulled the couple into a small conference room and identified herself as Naomi Sugar, an abuse and trauma consultant. She told them she had reviewed Nicholas’s case file and said, according to a summary she wrote later, “Inflicted trauma [is] the highest consideration at this time.” Sugar believed Nicholas had been abused.
Other than the lumbar puncture, the only thing the Felixes could think of that might explain the symptoms was that 11 days earlier Nicholas had slipped out of Nathan’s hands in the tub when Nathan gave him a bath. But in Sugar’s report the next day she wrote, “Rib fractures rarely result from falls.” She concluded with a statement that would forever change their lives: “Plan: Will speak with CPS and police when they arrive later today.”
It began with the monkeys.
The medical literature that would change the Felixes’ lives dates back to 1968. That’s when Dr. Ayub Ommaya, a professor of neurosurgery at George Washington University studying the role of whiplash on loss of consciousness, strapped rhesus monkeys into small sleds designed to glide down a track similar to the tracks used in crash-test dummy experiments. Ommaya and his team tied down the monkeys’ arms and legs but left their heads and necks unrestrained. Then they triggered a piston that slammed against the back of the sled, imitating a 40-mile-per-hour rear-end collision and causing the monkeys’ heads to violently whip back and forth.
When Ommaya conducted autopsies he observed that 15 of the 19 monkeys who lost consciousness had excess blood gathered between the outermost layer of their brains and the lining between their skulls and brains, a phenomenon known as subdural hematoma. Eight of those 19 also exhibited severe neck injuries.
After Ommaya published his findings in a 1968 issue of the Journal of the American Medical Association, British pediatric neurosurgeon Norman Guthkelch noted that subdural hematoma in patients under two years old was sometimes accompanied by a second symptom: bleeding behind the pupils (known as retinal hemorrhaging). Connecting Ommaya’s monkey experiments with his own observations, Guthkelch published a paper (“Infantile Subdural Haematoma and Its Relationship to Whiplash Injuries”) in the British Medical Journal in 1971. John Caffey, an American pediatric radiologist, followed that with his own in Pediatrics (“The Whiplash Shaken Infant Syndrome”) in 1974. Caffey and Guthkelch posited that a series of unexplained infant head injuries were in fact the result of covert, violent shaking by caretakers. The smoking gun became the triad of retinal hemorrhage, subdural hematoma, and a third symptom later introduced by other doctors, cerebral edema, or excess fluid in the brain.
By the 1980s “whiplash shaken infant syndrome” had become known as “shaken baby syndrome.” The Seattle Times got an early jump on the SBS scourge in 1981 with an article titled “The Boy Friend: A Growing Threat in Child Abuse” (in which we’re told that SBS often happens when a man is “baby-sitting with a child not his own…so there’s no real bond with the child. The baby squirms during changing or won’t shut up”).
From the mid-1980s to the early 2000s, SBS stood alongside other high-profile public scares like shark attacks or strangers with candy, reaching its media apex during the case of British au pair Louise Woodward, accused of shaking an infant to death in Newton, Massachusetts, in 1997.
The notion that SBS is more likely to stem from a caretaker other than the baby’s biological parent gained more traction in 1998, when Cayce Lee Brooks of Vancouver, Washington, was charged with shaking her adopted 10-week-old son. She denied the accusation and turned down a plea deal that would have reduced her sentence to three years. She refused “to spend time in prison for a crime I did not commit,” she told the court. The jury found her guilty and she was sentenced to nearly eight years in prison.
In 2002, also near Vancouver, prosecutors charged Heidi Fero of shaking 15-month-old Brynn Ackley, whom she was baby-sitting. Paramedics said they found the toddler unconscious with bruises on her face. Fero maintained that Brynn’s four-year-old brother had accidentally caused the injuries while playing too rough. A jury found Fero guilty of first-degree assault of a child. Brynn is now severely mentally disabled, and Fero is serving a 10-year sentence.
Throughout Washington state, according to data from the past 25 years collected by Northwestern University’s Medill School of Journalism, authorities have charged 57 people with violently shaking a child. In Seattle a leading expert on SBS for at least a decade was Naomi Sugar, the doctor who believed someone had shaken Nicholas Felix.
Sugar, the medical director of the Harborview Center for Sexual Assault and Traumatic Stress, had gained a national audience among child abuse experts for her 1999 position paper on bruising. She also helped write many of the state’s Department of Social and Health Service’s policies.
Translation: It was going to be Robyn and Nathan Felix’s word against that of one of the most respected child abuse experts in the state.
At midnight, October 25, 2008, a social worker at Seattle Children’s approached Robyn and Nathan and asked them to sign an agreement stating they would not leave the hospital with their son. The Snohomish County Sheriff’s department soon took custody of Nicholas—and subsequently transferred custody to a CPS-approved family friend in Fife, 50 miles south.
They could not have their son back until CPS had cleared them. This involved numerous consultations with social workers, all of whom, Nathan and Robyn felt, were convinced that Nathan had shaken Nicholas in a fit of rage. At one point, a caseworker confided to Robyn, If your husband would only admit what he has done, then I can put services into the home. Essentially: Admit that we’re right and all this will go away.
On the night of Friday, November 21, the couple put Eliana to bed and retired to bed themselves. Despite the upheaval of the past month, they were both, in their own way, at peace. They had spent weeks doing as CPS had asked, short of admitting to shaking Nicholas. They felt certain their son would be back in their arms soon. They drifted off to sleep around 10pm.
Thirty minutes later they awoke to a loud knock at the front door.
Though it didn’t halt the arrest of Nathan Felix on that cold night in November 2008, an active debate now in the medical community may lead to more clarity in alleged shaken-baby cases. Stanford pediatric radiologist Patrick Barnes, one of the experts called to testify in the trial of Louise Woodward, the British au pair, has raised doubts. Though Barnes testified against Woodward in the 1997 case, he has since changed his view. “When we started using more advanced imaging techniques such as MRI,” he told PBS’s Frontline in 2011, “we started realizing there were a number of medical conditions that can affect a baby’s brain and look like the findings that we used to attribute to shaken baby syndrome or child abuse.”
Those conditions include trauma during birth, accidental falls, brain infections, and vitamin D deficiency.
“If you look at it with any scrutiny whatsoever, the absolute bogus nature of the syndrome is clear as a bell,” Steven Gabaeff, a retired Sacramento-based ER doctor told me recently. Gabaeff, who worked in emergency medicine for 35 years and has practiced clinical forensic medicine for the past 25, says we’ve gotten it wrong since the beginning. In a 2011 Western Journal of Emergency Medicine article, he pinpointed the fallacy of using Ommaya’s 1968 experiment with rhesus monkeys as a biomechanical basis for SBS.
For one, no adult could possibly shake a baby with the force of a 40-mile-per-hour automobile impact. And even if they could, there would most likely be neck trauma, which almost half of Ommaya’s monkeys exhibited but supposed SBS victims rarely do. Second, John Caffey and Norman Guthkelch, the doctors who linked Ommaya’s results to the clandestine shaking of infants, did not take into account common birth trauma, a frequent source of subdural hematoma. Finally, maternal and prenatal vitamin D deficiencies, which also contribute to subdural hematoma and retinal hemorrhage, may lead to the kinds of bone fractures often associated with physical abuse.
“There has never been an eye-witness case of shaking in which the baby was taken to the hospital and evidence of subdural hemorrhage and retinal hemorrhage was found,” says Gabaeff, who frequently testifies in court about SBS.
Even Norman Guthkelch, now in his late 90s, questions its relevance in criminal cases. “The triad may legitimately be classified as a syndrome, but it is not necessarily the result of shaking, or of abusive behavior,” he recently wrote.
In the wake of overturned verdicts and dropped charges, proponents of the SBS hypothesis have begun to run from the term. Abusive head trauma is often used by even those organizations, such as the National Center on Shaken Baby Syndrome, with the old nomenclature in their names.
“I think that prosecutors are more willing to dismiss these cases now, before they ever get to a jury,” Deborah Tuerkheimer, the DePaul University law professor and Flawed Convictions author, told me. “I think that juries are more likely to find the defendant not guilty than they were five years ago. I think that even doctors are starting to look harder into other possibilities.”
You will lose your house. Consider it gone. Your savings, if you have any, will evaporate. Robyn Felix could not believe the audacity of the woman on the other end of the line. How could she say such things? Robyn had found the woman, a retired lawyer, after months of researching SBS. Amid a major discovery Robyn made online—that botched lumbar punctures can cause the symptoms Nicholas exhibited at Seattle Children’s—one name kept popping up in legal briefs and on SBS listservs: Heather Kirkwood. She had filed appeals in several cases involving men and women serving time for shaken baby syndrome convictions. When Robyn discovered that Kirkwood lived in Seattle, she tracked down her phone number and dialed.
She breathlessly told Kirkwood her story—Nicholas’s symptoms, Nathan’s arrest, how Nicholas and Eliana were back home but, months later, Nathan wasn’t. He had been released from jail after 48 hours but had to live in an apartment away from the children so CPS wouldn’t place them in foster homes.
Kirkwood, a former litigator for the Federal Trade Commission, got involved in criminal law for the first time while in her 50s, when her daughter-in-law’s brother was convicted of sexual assault in Texas. He was out on probation, and Kirkwood had to know if she could trust him around her family. She delved into his case, sending test results to doctors around the country, and ultimately decided that he was innocent. Her work overturned his conviction.
Soon another Texas man sought her help: Ernie Lopez, serving a 60-year sentence for raping and killing—via SBS—an infant girl in his care. Lopez maintained his innocence, and upon examining the case, Kirkwood and her cadre of doctors agreed and Lopez won his freedom with a plea deal for time served.
Robyn emailed all the documentation in Nicholas’s case to Kirkwood, who forwarded copies to medical experts, including Patrick Barnes, the Stanford radiologist who had changed his opinion about SBS after testifying for the prosecution in the Louise Woodward trial.
As Kirkwood predicted, the Felixes fell into debt. In addition to keeping up with the mortgage on the house, they had to pay rent for a room at a friend’s house, where Nathan, forbidden to live with his children, was forced to stay. He also took a leave of absence from the Air Force Reserves, resulting in loss of income. And because Nathan couldn’t be alone with the kids, the couple had to pay for day care, about $1,200 a month, when Robyn was at work.
Meanwhile, Robyn began exhibiting anxious behavior: “I started washing the dishes for hours a day, literally hours a day just washing the dishes over and over again.” Traumatized by the night the sheriff’s deputies took her daughter and husband, whenever she saw an unfamiliar car enter the neighborhood, she’d lock the door and turn off the lights, telling the kids to pretend they weren’t home.
In April 2009, Patrick Barnes submitted his opinion to Snohomish Superior Court. He reviewed Naomi Sugar’s evaluation of Nicholas, noted both the birth mother’s drug use and the lumbar punctures, and concluded, “The radiology findings are consistent with the child’s history and appear to be natural and/or accidental in nature, with no indicators of non-accidental trauma.” In other words, Barnes believed Sugar got it wrong.
Heather Kirkwood tells me to shake the baby. “Go ahead, give it a good hard shake,” she says in her basement office lined with binders of dozens of child-death case files. The infant, clad in a pink onesie, feels like a plush bag of flour in my hands, a doe-eyed expression stamped into its plastic face: the official demonstration doll from the National Center on Shaken Baby Syndrome.
Kirkwood tugs the doll from my grip, hooks her hands under the armpits, and shakes it six or seven times with so much force the head flaps against its back and chest. That’s the amount of force required to cause shaken baby syndrome, she says.

Truth Seeker Retired attorney Heather Kirkwood studies shaken baby syndrome cases and files appeals pro bono from her Seattle home. She also connects clients like Nathan and Robyn Felix with medical and legal experts.
Image: Robin Stein
Wouldn’t that break a real infant’s neck? “Yes, exactly.” Just like the monkeys in Ommaya’s 40-mile-per-hour-impact experiment.
More dolls of various shapes are piled in a corner, along with a bassinet and a stroller. And the binders: hundreds of them stacked not only in the basement but all over the house—in a guest room, atop the kitchen table. Hole-punched between the covers are police investigations, appeals briefs, and autopsy reports. The people in the binders hail from all over the world. She performs all the work pro bono, filing appeals and serving as a facilitator between the accused and the medical experts who might be able to help them.
When I ask Kirkwood what cases she’s working on these days, she fires up a desktop computer in the basement. In her inbox: at least 20 new emails from all over the world. Click. “This guy is from Sweden,” she says. “Tragic case, totally innocent.” Click. “Oh no, this guy is getting life. He didn’t do it.” Click.
I ask why so many of her clients are men. “There’s certainly a tendency for investigators to suspect men over women,” she says, but “the police follow whomever the doctors tell them to. So if the doctors tell them that Mother Teresa was the last person with the child and must therefore have been the one that violently shook the child, then Mother Teresa it is.”
Everything Kirkwood told Robyn Felix in that first phone call came to pass. The bank foreclosed on the house and the family nearly went bankrupt. But after living apart for 257 days, Nathan and his wife and kids were allowed to live in the same home. Thanks to the statements by Kirkwood’s experts and other doctors—including psychiatrists who evaluated Robyn and Nathan—the Department of Social and Health Services dropped the case in July 2009. Broke, the family moved to Gainesville, Florida, where Robyn’s sister lives, and where they both found jobs in health care.
And Nicholas? He’s fine. After everything, he’s a healthy, normal kid, Robyn told me in May 2013 by phone from Florida. He was turning five soon. He has blond curly hair “like a little cherub,” Robyn said. “But he’s got this devilish grin.” He likes salt-and-vinegar potato chips. He likes bugs. “There’s no shortage of those here,” she laughed.
I had planned to end the story there.
A week following my conversation with Robyn, a Seattle lawyer contacted me to say that Robyn and Nathan Felix would no longer talk to me. The couple had filed suit against Child Protective Services, DSHS, and Group Health for damages, and the lawyer asked Seattle Met to hold the story because it might hurt their chances in court. I didn’t want to be the source of more hardship for the family. After a conversation with my editor, I reluctantly obliged.
Still, every month or so I’d check in on the case—unable to get the Felix family and the controversy surrounding shaken baby syndrome out of my head. During one Google search I came across a Seattle Times article with the headline, “Dr. Naomi Sugar, Who Worked with Abused Children, Dies at 62.” The doctor who first suspected Nicholas Felix was abused had died of ovarian cancer on July 20.
I had never thought of Sugar as the villain in the Felixes’ story. While it seemed she had gotten it wrong in this case I had always assumed she was doing her job based on the best science she believed was available.
I came across an obituary page dedicated to Sugar, along with a video clip made on the occasion of her recent retirement. Dozens, maybe even a hundred Harborview, Seattle Children’s, and prosecutors’ office employees gushed about their love for Naomi Sugar. Many of them talked about the children whose lives she had changed for the better.
In December 2013 I got an email from Nathan Felix. The lawsuit had been settled out of court. The family received $55,000, just enough to cover legal costs. I called Nathan and asked what he thought of the outcome. No, the court settlement won’t be enough to dig him out of his financial hole, but he has no interest in pursuing the case further. The family is still together and that’s all that matters to him. He hadn’t heard about the death of Naomi Sugar, and when I told him, he fell silent.
In the background I could hear Nicholas, now almost six years old, and his sister Eliana, seven, roughhousing. The cherub and the princess. Their voices grew louder and louder—the kind of childhood laughter that rises to a falsetto pitch—until their father held the phone away from his mouth and called out in a calm and even tone.
“Please be quiet. I’m trying to talk.”

The Felix Family (clockwise from top left) Nathan, Robyn, Eliana, and Nicholas




